Medical compression spandex refers to high-elastane textile materials engineered to apply therapeutic pressure on the body. These fabrics are fundamental in healthcare garments – from compression socks to surgical binders – where controlled, graduated pressure can improve circulation and support healing. In this guide, we explore what high-compression spandex is, its composition and construction, and how it’s used in medical applications. We also detail the technical attributes (like pressure ratings in mmHg, stretch and recovery, breathability, etc.) that define medical-grade compression fabrics.
A classification guide (Classes I–IV) is provided to link compression levels with recommended fabric characteristics. Finally, we offer tips for selecting the right medical compression spandex fabric based on use case, skin sensitivity, layering needs, and targeted compression zones. The aim is to provide a professional, technical overview suitable for healthcare product developers, medical textile manufacturers, and therapeutic garment designers.
What is High-Compression Spandex?
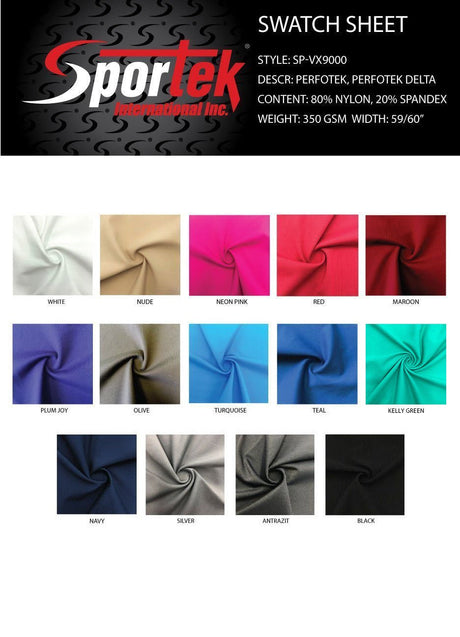
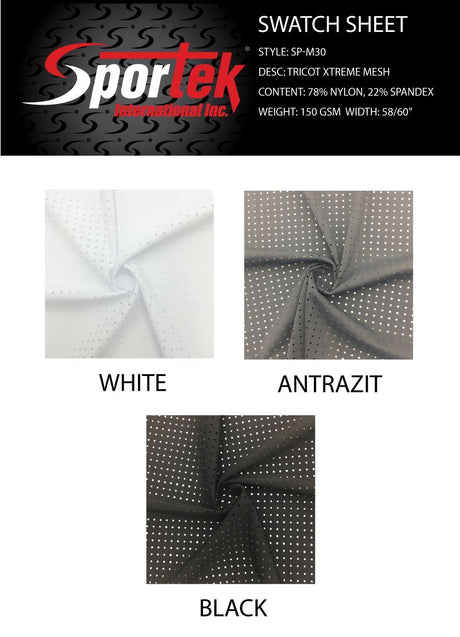
High-compression spandex fabric is a textile that contains a significant percentage of elastane (spandex) fibers, allowing it to stretch and exert substantial compressive force on the body. Typically, these fabrics are blends such as nylon/spandex or polyester/spandex, often with 15–30% spandex content. The non-elastane portion (nylon or polyester) provides strength and durability, while spandex provides elasticity.
Notably, nylon (polyamide) is often preferred for medical compression due to its smoother texture, high strength, and superior moisture management (nylon can wick moisture roughly three times more effectively than polyester). An industry comparison found that an 80/20 nylon-spandex blend (80% nylon, 20% spandex) can deliver firm 4-way stretch compression (holding about 25 mmHg of pressure) with about 92% recovery (meaning it nearly returns to original length after stretching), and high abrasion resistance (tolerating ~50,000 cycles). In contrast, comparable polyester-spandex blends may show lower elastic recovery (~75%) and can degrade (yellow) under UV exposure. This highlights why medical compression spandex fabrics often use nylon-spandex power yarns to achieve reliable, long-term compression power and resilience.
Stretch Levels and 4-Way Elasticity: High-compression fabrics are engineered for significant stretch in all directions (4-way stretch). This ensures the material can conform snugly around complex body contours and exert even pressure. A quality medical compression fabric might elongate 150–250% in length and width while still “recovering” to its original size. The knitting technique plays a major role in controlling stretch: warp-knit constructions are commonly used for compression fabrics because they produce a more stable, less stretchy structure ideal for consistent, strong support.
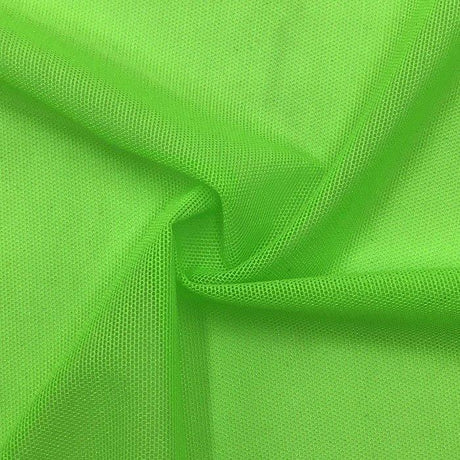
Warp knitting (using interlocking loops running lengthwise) yields fabrics with controlled elasticity and excellent recovery that maintain consistent compression over time. Examples include powernet and power mesh fabrics used in medical and shapewear products. Powernet, for instance, is a tightly knitted mesh (usually nylon/elastane) known for significant support and compression; its firm elasticity makes it ideal for areas requiring high control (like post-surgical binders or compression bra bands). Despite its firmness, powernet’s open mesh structure makes it breathable, and it is prized for durability – holding its shape and compression level even with prolonged wear. Power mesh is a lighter variant: also a warp-knit nylon/spandex mesh but with a looser knit. It has greater stretch and drape, offering gentler compression – useful as a lining or for mild support in less critical areas.
In contrast to warp knits, weft-knit (circular knit) fabrics have higher stretch and a softer feel but less inherent power. Weft knits (like those used in athletic leggings) are extremely elastic in all directions but tend to provide lower, more uniform compression and may gradually lose shape if not reinforced. For medical compression spandex applications, warp-knit fabrics (e.g. tricot powernets) or hybrid constructions are favored to achieve the required high tension and long-term shape retention.
Construction Methods: Common construction methods for high-compression spandex fabrics include circular knitting (producing seamless tubes like compression stockings) and cut-and-sew from warp-knit yardage (for custom garments with panels). Circular-knitted compression stockings are typically seamless and provide graduated compression by varying stitch tension during knitting. Flat-knit (cut-and-sew) garments allow creation of different panels with varying stretch properties; for example, a garment might incorporate a high-compression powernet panel at an abdominal section and a lighter stretch fabric elsewhere to create zones of differing compression. Some advanced designs use targeted compression zones by sewing in panels of stronger fabric in specific areas to reinforce compression.
However, adding too many seams or panel transitions can cause discomfort or chafing, so designers balance targeted support with patient comfort. Overall, high-compression spandex fabrics are defined by their high elastane content, engineered knit structures (warp knit powernet, supportive interlocks, etc.), and the ability to exert a specific pressure profile on the body without permanent deformation.
Medical Uses of Compression Fabrics
High-compression spandex materials are used to fabricate a variety of medical and therapeutic garments. These medical compression spandex applications take advantage of controlled pressure to achieve health benefits:
• Post-Surgical Garments: After surgeries (e.g. orthopedic procedures, abdominal surgery, liposuction or other plastic surgery), patients often wear compression garments to support tissues and reduce swelling. These garments (such as abdominal binders, compression vests, or girdles) promote circulation and reduce edema and bruising, which aids healing. By applying uniform pressure over the surgical area, they help prevent fluid buildup (seromas) and provide gentle support to incisions, potentially lowering risk of wound complications. Medical compression spandex fabrics used here must balance firm support with comfort for continuous wear.
• Lymphedema Sleeves and Garments: Lymphedema (often in the arm after lymph node removal, or in legs) is managed with compression to encourage lymph fluid drainage. Compression sleeves or stockings for lymphedema are usually made of strong, stiff elastic fabrics that provide graded pressure (highest at the distal end) to push fluid out of the swollen limb. These may be custom flat-knit sleeves for severe cases (providing higher compression and containment for irregular limb shapes) or circular-knit for milder edema. The goal is to prevent fluid accumulation and stimulate lymphatic return, so the spandex fabric must sustain a therapeutic pressure (often Class II or III compression) throughout daily activity. Fabrics are chosen for durability and stiffness (to create high working pressure – see technical section on “stiffness”) as lymphedema garments often face prolonged use.
• Varicose Vein and Venous Insufficiency Support: Perhaps the most common use of compression spandex is in compression stockings for chronic venous disorders (varicose veins, chronic venous insufficiency). By applying external pressure on the legs, these stockings help vein valves function and prevent blood pooling. Medical compression stockings (typically knee-high or thigh-high) are knit to deliver graduated compression (strongest at the ankle, decreasing upward) which improves venous return. Mild cases or preventive use (e.g. for long travel or standing all day) might use Class I (15–20 mmHg) stockings, whereas pronounced varicose veins or venous ulcers require Class II or higher (20–40+ mmHg) support as prescribed. The spandex in these stockings is often double-covered yarn (spandex wrapped in nylon) to increase longevity and ease of donning. These fabrics also need good moisture wicking and anti-microbial properties because stockings are worn for long hours daily.
• Orthopedic Bracing and Support: Compression fabrics are integrated into orthopedic supports like knee braces, ankle sleeves, or back supports. High-compression elastic panels provide joint stabilization and reduce swelling in injuries. For example, a knee compression sleeve made of a heavy nylon-spandex knit can provide joint proprioceptive support and limit edema after a sprain. Braces may combine inelastic components (straps, hinges) with power spandex panels that conform to the body. Here the medical compression spandex must be robust (withstanding repetitive movement) and often has a 4-way stretch so it doesn’t restrict range of motion while still applying pressure. Orthopedic compression fabrics may feature specialized knit patterns (e.g. patella relief zones) and often have breathable or perforated sections for comfort.
• Burn Scar Management: In burn therapy, custom pressure garments made of high-compression spandex fabric are crucial for scar management. These garments (often full body suits, gloves, face masks, etc., made to patient measurements) apply continuous pressure to healing burn wounds or grafts to flatten hypertrophic scars and improve scar appearance. Research and clinical practice suggest that maintaining a pressure around 20–30 mmHg on a maturing scar for 23+ hours a day can significantly reduce excessive scar tissue formation. Burn compression garments are typically made from powernet or strong Lycra®-type fabric that can deliver this pressure uniformly. The fabric must have a high elastane content and six-way stretch to contour over complex body areas (e.g. fingers, face) without causing pressure gaps. They also need to be soft on the skin and breathable, since they’re worn on fragile healing skin for long durations. Advances include moisture-wicking and cooling variants (e.g. CoolMax® blended compression fabrics) to improve patient comfort while still providing ~17–24 mmHg compression in lightweight form.
• Diabetic Circulation Aids: People with diabetes may use mild compression socks or sleeves to improve circulation in the legs and feet. While compression must be used cautiously in diabetics (due to risk of pressure injury if neuropathy is present), medical compression spandex socks in the 15–20 mmHg range are sometimes recommended to reduce edema and enhance blood flow in those with venous insufficiency or mild swelling. These diabetic support socks are usually made from softer, seamless knit fabrics (often with added cotton or anti-microbial fibers like silver) to minimize friction and moisture, addressing diabetic skin sensitivity. The compression helps prevent blood pooling and reduces minor edema, which in turn can aid in preventing ulcers. It’s crucial such garments are properly fitted and of medical-grade quality, as too loose they won’t help, and too tight could impede circulation. (Note: In severe arterial disease, compression is contraindicated – so selection should follow medical advice.)
(Other uses: Medical compression fabrics are also found in DVT prophylaxis sleeves (e.g. T.E.D. stockings ~18 mmHg used in hospital to prevent clots), maternity support belts, and dynamic compression devices, but the above are the primary applications in scope.)*
Technical Attributes of Medical-Grade Compression Fabric
Several technical attributes differentiate medical compression spandex fabrics from ordinary stretch fabrics. These characteristics ensure the fabric can provide therapeutic pressure while remaining wearable and safe for patients:
• Pressure Rating (mmHg): Medical compression fabrics are classified by the pressure (in millimeters of mercury) they exert on the body. This mmHg pressure rating is essentially the “strength” of compression. Medical-grade compression usually starts at around 20 mmHg or above – pressures at this level and higher are considered therapeutic and often require professional fitting. The pressure is measured using specialized instruments that simulate the limb circumference; manufacturers knit or calibrate the fabric tension so that at a given stretch, it delivers the target mmHg. For example, a Class II fabric might exert ~30 mmHg when stretched to fit an average ankle circumference. Accurate pressure calibration is critical: too low and the garment won’t be effective, too high and it could impair circulation. Thus, quality control testing is done to ensure each production batch meets the mmHg specifications (see “Testing and Standards” section for how this is certified).
• 4-Way Stretch and Elastic Modulus: Medical compression textiles have high multidirectional stretch. 4-way stretch means the fabric can extend both widthwise and lengthwise significantly. This allows garments to be donned and to conform to body curves while maintaining even pressure. The elastic modulus (stiffness) of the fabric is engineered so that it offers strong resistance as it stretches – this resistance is what generates pressure against the body. High-compression spandex fabrics often use knit structures that provide graduated elasticity: tighter (higher tension) in one area and slightly more forgiving in another, enabling gradient compression profiles. The fabrics also exhibit excellent elastic recovery – the ability to spring back after stretching – which is crucial for maintaining compression over repeated uses. A medical-grade compression fabric will typically recover a high percentage of its original length (e.g. >90% recovery) to avoid “stretching out” with wear.
• Strong Recovery and Fatigue Resistance: Recovery refers to how well the fabric returns to its original shape after stretch, and fatigue resistance refers to how many cycles of stretch the fabric can endure before losing elasticity. Medical compression garments are worn daily and stretched repeatedly (with each movement of the body), so the fabric must not quickly “relax” or lose compression. Quality compression spandex is made with durable elastane (often double-covered yarns to protect the elastic core) to achieve thousands of stretch cycles with minimal degradation. For instance, warp-knit powernet fabrics are known for maintaining their compressive force over time – they resist elongation and don’t suffer runs or tears easily. Fabrics are lab-tested for cycle strength (e.g. via abrasion and extension testing); a high-grade fabric might withstand tens of thousands of stretch cycles (as noted, ~50k cycles in lab tests for some nylon/spandex powernets) before significant loss of compression.
• Breathability and Moisture Management: Because compression garments fit tightly and may be worn for extended periods, breathability and moisture-wicking are key. Medical compression spandex fabrics often incorporate microfiber nylon or special polyester (e.g. CoolMax®) to pull sweat away from the skin and allow airflow. The knit structure (like mesh or ribbing) can also enhance ventilation. Good moisture management prevents skin maceration and discomfort – a dry, breathable garment reduces itchiness and bacterial growth. For example, a compression sleeve may use a moisture-wicking finish or yarn that dries quickly, keeping the limb cool. Some modern medical fabrics have thermoregulating properties – they might be engineered to be insulating when cool and cooling when hot, aiding comfort in various climates.
• Anti-Microbial and Skin-Friendly Finishes: Given the close-to-skin, prolonged wear nature of these garments, many medical compression spandex fabrics include anti-microbial treatments. Silver-ion or zinc treatments, or inherent yarn properties (like bamboo-charcoal or copper-infused fibers), can inhibit bacteria and fungus growth, reducing odor and risk of infections (important for diabetic users or those wearing bandages). Additionally, fabrics are often tested for biocompatibility – they should be latex-free (to avoid latex allergy issues) and may be certified to OEKO-TEX® Standard 100 (meaning they contain no harmful substances).
“Skin-friendly” compression fabrics might also incorporate aloe or vitamin E micro-capsules for moisturizing effect, though typically in consumer-grade items; for medical grade, the focus is on inert, hypoallergenic materials. Softness is also a factor: the fabric’s finish should minimize seams and roughness. Some manufacturers offer silicone-coated yarns or special knitting techniques to make the inside surface smoother, since fragile or sensitive skin (as in burn patients) can be easily irritated. In summary, a top-quality medical compression fabric couples high performance (pressure and stretch) with patient comfort features like breathability and antimicrobial protection to enable safe, continuous use.
• Graduated Compression & Fabric Design: A hallmark of medical compression garments (especially for limbs) is graduated compression – higher pressure distally, easing proximally. While this is more of a garment design aspect than a raw fabric property, it’s achieved through the fabric’s knit pattern and tension settings. For example, a circular knit compression stocking is programmed so that the spandex tension is highest at the ankle and gradually lower up the calf.
In flat-knitted panels, the designer might choose a higher modulus fabric for the lower part of a sleeve and a slightly more elastic one for the upper part, or simply shape the pattern to achieve a looser fit upward. The ability of a compression fabric to be engineered or combined to create these pressure differentials is a key attribute. Fabrics used must respond predictably to stretch – which is why standardized elastic testing is done (measuring force at various elongations) to ensure a given material will deliver, say, 30 mmHg at 50% stretch and taper to 20 mmHg at 20% stretch, etc. This reproducibility is crucial for meeting medical compression standards.
Compression Classes and Fabric Characteristics
Medical compression garments are grouped into compression classes based on their pressure level (mmHg). Below is an overview of Classes I–IV, including typical pressure ranges and recommended fabric characteristics for each class:
| Compression Class | Pressure Range (at ankle) | Recommended Fabric Characteristics |
| Class I (Light) | 18–21 mmHg |
Soft, highly elastic fabric with moderate spandex content (e.g. ~15–20% elastane). Often a lightweight circular knit or smooth warp-knit that is easy to don and comfortable for all-day wear. Emphasizes breathability and softness for mild compression needs (ideal for early varicose veins, mild edema, or preventive wear). |
| Class II (Moderate) | 23–32 mmHg |
Stronger fabric with higher elastane (often 20–30% spandex) and firmer stretch. Warp-knit powernet or tight circular knit used to ensure consistent moderate pressure. Fabric should have excellent recovery and durability (to sustain ~25–30 mmHg) yet still allow 4-way stretch for ease of movement. Typically medium-weight, with good moisture wicking. Used for moderate varicose veins, post-surgery swelling, and many lymphedema cases. |
| Class III (Strong) | 34–46 mmHg |
Heavy compression fabrics, usually warp-knitted with high elastane or even layered construction. These fabrics are high-stiffness (low stretch) to provide a high level of containment. Often custom-made flat knit garments are in this class. Fabric may be thicker or have a rigid structure (while still elastic), to exert ~40 mmHg without excessive stretch. Strong nylon-spandex blends (sometimes >30% spandex) with reinforced seams or panels are common. Used for severe edema, lymphedema Stage II–III, or significant venous insufficiency. |
| Class IV (Very Strong) | ≥ 49 mmHg |
Extremely firm compression, generally reserved for advanced lymphedema or unusual cases. Fabrics here are highly specialized – very dense knits or multiple layers of compression fabric. They have minimal stretch beyond what is needed to put the garment on, ensuring maximum pressure. The material might be a heavyweight powernet or a combination of non-elastic fabric + elastic panels to reach pressures 50 mmHg and above. Only custom garments (made-to-measure) achieve Class IV, and they must be carefully engineered to avoid cutting off circulation. These fabrics prioritize support over comfort, though they still must be breathable and skin-safe. |
Note: The above classes correspond to the widely used German RAL standard (also adopted in many regions) where Class I–IV are defined by those mmHg ranges. In the French Afnor system or some US conventions, class naming can differ, but the concept of increasing pressure remains the same. Regardless of class, all medical compression spandex fabrics must deliver a controlled, gradually decreasing pressure from the distal to proximal end to be effective. Fabric selection for each class hinges on balancing the required strength (higher classes need stiffer, stronger fabrics) with wearability (lower classes favor softer, finer materials for comfort).
Selecting the Right Compression Fabric
Choosing the appropriate medical compression spandex fabric for a project involves considering the medical purpose, patient needs, and practical garment construction. Here are key tips and factors to guide selection:
• Match Fabric to Intended Medical Use: The condition or therapy will dictate the compression class and thus the fabric requirements. For example, designing a post-surgical compression vest (for edema control after surgery) might call for a moderate Class II fabric that is breathable and easy to don, whereas a garment for managing burn scars or stage II lymphedema might require a firmer Class III fabric to provide higher sustained pressure.
Always select a fabric capable of safely delivering the needed mmHg range for the target use. If the use is long-term chronic wear (like lymphedema), durability and consistent compression over time are top priority. For short-term or prophylactic uses (e.g. travel socks for DVT prevention), you might prioritize comfort and ease of use in a Class I fabric. In summary, align the fabric’s compression power and characteristics with the therapeutic goals (mild support vs. high containment, temporary use vs. daily long-term use, etc.).
• Consider Skin Sensitivity and Comfort: Patients who wear compression garments often have sensitive skin (for instance, post-surgery or burn patients, or people with neuropathy). Selecting a fabric with a soft touch and skin-friendly properties is crucial. Look for microfiber nylon or cotton-blend compression fabrics if the patient has tactile sensitivity – these tend to feel softer and cooler on the skin. Ensure the fabric is latex-free and ideally has been tested for irritants (many medical compression textiles come with certifications or at least material safety data).
If the garment will be worn in warm climates or by an active person, moisture-wicking and breathable fabric is a must – consider those with mesh constructions or moisture-management finishes. For example, a diabetic compression sock might use a bamboo charcoal nylon-spandex fabric that is naturally antibacterial and soft. Also, check if the fabric has flat, smooth surfaces on the skin side to minimize friction. Some high-compression fabrics have a slight sheen or slick feel (due to high-density knit), which actually can help when pulling the garment on and reduce friction on skin. Overall, never sacrifice patient comfort: a slightly lower compression that the patient will actually wear consistently is more effective than a higher compression fabric that is too uncomfortable and ends up not being used.
• Layering and Garment Design Requirements: Think about how the compression fabric will be used in the final product. Will it be a single-layer garment or part of a multi-layer system? If the compression is combined with foam pads or bandages (common in lymphedema management), the fabric needs to be robust enough to compress over those and possibly have less stretch (to provide additional stiffness). If the garment will be worn under regular clothing, a thinner profile and low-friction exterior (to slide under clothes) might be important – many medical hosiery fabrics have a smooth knit that won’t catch on pants. Conversely, if you are designing a brace with an elastic panel, you might choose a plush backed elastic fabric for comfort against skin and to prevent sliding.
Consider also the donning/doffing needs: higher compression classes can be very difficult to put on, so fabrics with a bit of surface slip (silky feel) or using a two-way stretch (stretch in one direction to assist pulling up, but stable in the other for compression) might be strategic. Some designers incorporate zippers or hook-and-loop closures in high-compression garments; in those cases, make sure the fabric can handle sewing and the stress concentration near closures (reinforced powernet might be needed around a zipper area, for example). If layering garments (like wearing a compression sleeve under a pneumatic pump sleeve, or two compression stockings for extra high compression), ensure the fabric is breathable enough to prevent overheating and that seams or edges are thin to avoid pressure points.
• Desired Compression Zones and Paneling: When a garment needs variable compression in different areas (e.g., a higher-compression panel over an abdomen or a reinforced knee zone in a stocking), you have a couple of options. You can select a single fabric that has graduated knit tension built-in (common in round-knitted gradated stockings), or design the garment with different fabrics for different panels. If choosing the latter, pair fabrics that have compatible stretch characteristics to avoid mismatch at the seam. For instance, you might use a heavy powernet (strong compression) for the front panel of a post-liposuction abdominal binder, but a slightly lighter-weight power mesh at the sides for comfort and flexibility.
Sewing them together creates targeted compression zones. Ensure that transitions are smooth and won’t cause a tourniquet effect at the seams. Modern warp knitting technology even allows integrating different modulus zones in one fabric, but if that’s not available, the cut-and-sew panel approach works. Just remember: every seam is a potential point of irritation, so use flatlock or covered seams and possibly add a thin lining under seam lines for high-compression garments. When selecting fabrics for panels, also consider color and thickness differences if the garment should look uniform – sometimes a slightly lighter compression fabric can be doubled up in certain spots rather than introducing a completely different material, to achieve a similar effect.
• Compliance with Standards and Verification: Especially for medical devices, you should choose fabrics from reputable suppliers who provide data on compression performance and have certified quality standards. Look for compression fabrics that come with documentation of their pressure ratings (mmHg) at various stretches or sizes. Many medical textile suppliers will offer testing data – for example, using a HATRA or MST compression tester – showing that the fabric, when made into a certain circumference, yields the expected pressure. If you’re developing a product that needs regulatory approval or clinician acceptance, using a proven fabric that meets standards (such as RAL Grade compression or ISO certifications) can save a lot of validation effort.
Additionally, consider if the fabric complies with any specific regulatory guidelines (FDA, EU MDR) for medical textiles. In the U.S., while fabrics per se aren’t “FDA approved,” the finished compression garment will fall under FDA Class I or II medical devices. Working with fabrics that established medical brands use (and that pass their quality control) is a good practice. Always obtain samples and perform your own stretch/pressure tests on a mannequin or on human subjects to verify that the fabric choice actually achieves the design goal. Compression performance can be affected by sewing, garment size, and wear over time, so factor those in. In summary, due diligence in fabric selection – considering both user needs and regulatory requirements – is essential to create a safe and effective medical compression product.
Measurement, Testing, and Standards
Medical compression fabrics and garments undergo rigorous testing to ensure they deliver the prescribed pressure and are safe for therapeutic use. Key points regarding measurement and standards include:
• Measuring Compression (mmHg): Compression levels are quantified in millimeters of mercury (mmHg), the same unit used for blood pressure. Manufacturers measure this by simulating the garment on a leg or arm model with known circumference and using pressure sensors. For example, a compression sleeve labeled 20–30 mmHg should exert between 20 and 30 mmHg at the wrist/ankle of a standard size, tapering upward. To achieve this, each medical compression spandex garment is engineered with precise knit tension – as noted earlier, a 20–30 mmHg graduated arm sleeve will have ~20–30 mmHg at the wrist (distal point) and then a few mmHg less at the mid-arm, and so on.
Manufacturers use devices like the HOSY (Hohenstein System) or MST compression tester to verify the pressure profile on finished garments. It’s also common to test static pressure (resting pressure) as well as dynamic pressure; dynamic or working pressure reflects the increase when muscles flex under the garment. This relates to fabric stiffness: a stiffer fabric (higher modulus) will produce a higher surge in pressure during movement, which can be beneficial for venous return. Testing protocols ensure that even during movement, the pressure stays within safe bounds and that gradient is maintained.
• Certification and Standards (RAL, ISO, etc.): In Europe, the RAL-GZ 387/1 standard is a well-known guideline for medical compression stockings. If a stocking meets RAL’s stringent requirements (correct pressure in each class, a defined pressure drop from ankle to thigh, material durability, etc.), it earns a RAL quality mark. This gives clinicians and patients confidence that the product performs as labeled. Similarly, the French Afnor standard and British Standard have defined classes and testing methods for compression hosiery.
On an organizational level, manufacturers of medical compression textiles often adhere to ISO 13485 (medical device quality management) to ensure consistent production. There are also ISO test methods for textile elasticity and sustained pressure. Another important concept is OEKO-TEX® or skin contact standards – since these garments are worn next to skin, many products are certified to be free of harmful chemicals. Some countries or hospital systems require that compression garments be latex-free and biocompatibility tested (ISO 10993) if used on broken skin (as in burn patients). While not all compression fabrics will individually have an ISO certification, using materials that meet general safety textiles standards is advisable.
• FDA and Regulatory Guidelines: In the United States, compression garments intended for medical use are regulated by the FDA, typically as Class I medical devices (low to moderate risk). Class I devices (like most compression stockings, sleeves, etc.) are often exempt from pre-market notification (510k), but they still must be manufactured under a quality system and proper labeling. The FDA expects that these garments “provide the compression level claimed” and are not misbranded. Some higher compression or specialized devices (e.g. compression devices for treating edema via pumps) can fall under Class II with additional controls.
For fabric selection and testing, this means you should maintain documentation of the garment’s performance. FDA doesn’t “approve” fabrics, but if your garment is audited, you’d need to show it consistently meets the therapeutic claims. Leading compression brands list their products with FDA and perform lot testing to ensure compliance. Additionally, for insurance coverage, garments often need to meet standards: for instance, Medicare/HCPCS coding might differentiate gradient compression garments from non-medical ones. Adhering to recognized standards (RAL class, etc.) helps in these certifications and reimbursements.
• Quality Control – Ensuring Consistency: Producing medical compression garments is a precise process – any variation in yarn, knit, or finishing can alter compression. Thus, quality control tests are done on the fabric and finished product. Fabrics might be tested for elongation force at various points (to ensure the elastic modulus hasn’t deviated). Garments are often randomly pressure-tested from production lines. Because of these efforts, medical compression garments tend to cost more than consumer “athletic compression” gear.
The specialized knit structures and extensive testing (every roll of fabric may be stretched and checked, every lot calibrated) add to cost. However, this is necessary to guarantee therapeutic efficacy. When selecting a fabric supplier, look for one that can provide test data or certification for medical use. Many suppliers will offer to knit a sample to your specifications and provide a pressure curve graph. It’s wise to verify such data with independent testing if possible, especially for novel fabrics or very high compression classes.
In summary, medical compression spandex materials operate in a regulated context where accuracy and safety are paramount. By understanding and utilizing the standards (like compression class definitions, RAL quality marks, and FDA guidelines) and by rigorously testing fabrics for mmHg delivery, one can ensure that the end product truly benefits the patient as intended. This blend of materials science, engineering, and compliance is what elevates a piece of stretchy fabric into a trusted medical device.
Conclusion
High-compression spandex fabrics are the backbone of many therapeutic garments – providing healing support from the operating room to everyday living with chronic conditions. By blending elastane with high-strength fibers in smart knit constructions, these medical compression spandex textiles achieve something remarkable: they apply controlled, measurable pressure to the human body in a comfortable and wearable form. In this guide, we defined high-compression spandex and examined its compositions (nylon vs. polyester blends, warp knit powernets, etc.), delved into the spectrum of medical uses (from post-surgical recovery to lymphedema and beyond), and outlined the technical attributes that make a fabric “medical grade” (pressure ratings, 4-way stretch, recovery, moisture control, antimicrobial features). We also provided a classification of compression levels with guidance on suitable fabrics for each class, and offered practical tips on selecting fabrics tailored to specific needs, taking into account patient comfort and garment design considerations. Lastly, we emphasized how compression levels are measured and standardized, underscoring the importance of compliance with established medical standards and quality testing in this field.
Designing or choosing a compression fabric is a balancing act between technical performance and human factors. A medical compression spandex fabric must deliver the right pressure (and prove it via standards) while also being something a patient can tolerate wearing daily. With advances in textile technology – such as new moisture-wicking fibers, 3D knits for variable compression, and ever more durable elastanes – today’s compression fabrics are more effective and comfortable than ever.
For professionals developing healthcare products, understanding the nuances of these materials will enable creation of garments that improve patient outcomes, whether it’s a sleeve that controls lymphedema swelling or a surgical garment that speeds healing. In all cases, the ultimate measure of success is a fabric that meets medical objectives and earns patient compliance through thoughtful design. Armed with the information in this guide, developers and designers can more confidently specify the right high-compression spandex fabrics to achieve that goal – marrying science and comfort in life-changing medical textiles.